In healthcare, communication isn't just about being polite. It’s a core clinical skill that directly shapes patient safety, builds trust, and ultimately determines treatment outcomes. Think of it as the lifeline of patient care—a clear and compassionate exchange of information between healthcare professionals, patients, and their families, ensuring everyone is on the same page.
Why Great Communication Is a Clinical Skill
Let's get one thing straight: communication is not a "soft skill." It’s a critical competency. Whether you're in a busy hospital ward or a local GP's office, the quality of dialogue is just as vital as an accurate diagnosis. It's the connective tissue holding the entire patient care system together, ensuring vital information flows correctly between every single person involved.
When communication is handled well, patients feel heard, respected, and confident enough to take an active role in their own care. This creates a partnership built on trust, which is absolutely essential if patients are to stick with their treatment plans. On the other hand, when communication breaks down, the results can be devastating.
The Real-World Impact of Miscommunication
Poor communication isn't a small problem; it's a massive patient safety risk with staggering financial and human costs. In fact, failures in communication are a leading cause of harm that could have been prevented.
A landmark study analysing over 23,000 medical malpractice claims discovered that communication failures were a factor in more than 7,000 cases. These breakdowns contributed to nearly 2,000 preventable deaths and $1.7 billion in malpractice costs.
What’s more, it’s estimated that a shocking 80% of serious medical errors are tied to miscommunication between clinicians during patient handovers—a routine, yet incredibly high-stakes, process. These numbers paint a sobering picture of how quickly a simple misunderstanding can spiral out of control. You can explore more about the effects of poor communication in healthcare to grasp the full scale of the issue.
The Pillars of Clinical Dialogue
So, what does good communication actually look like? It’s far more than just talking. It's a multi-layered skill that requires a constant, conscious effort to connect and clarify. At its heart, it rests on a few key pillars.
The diagram below breaks down Active Listening, a central pillar, into its core components.
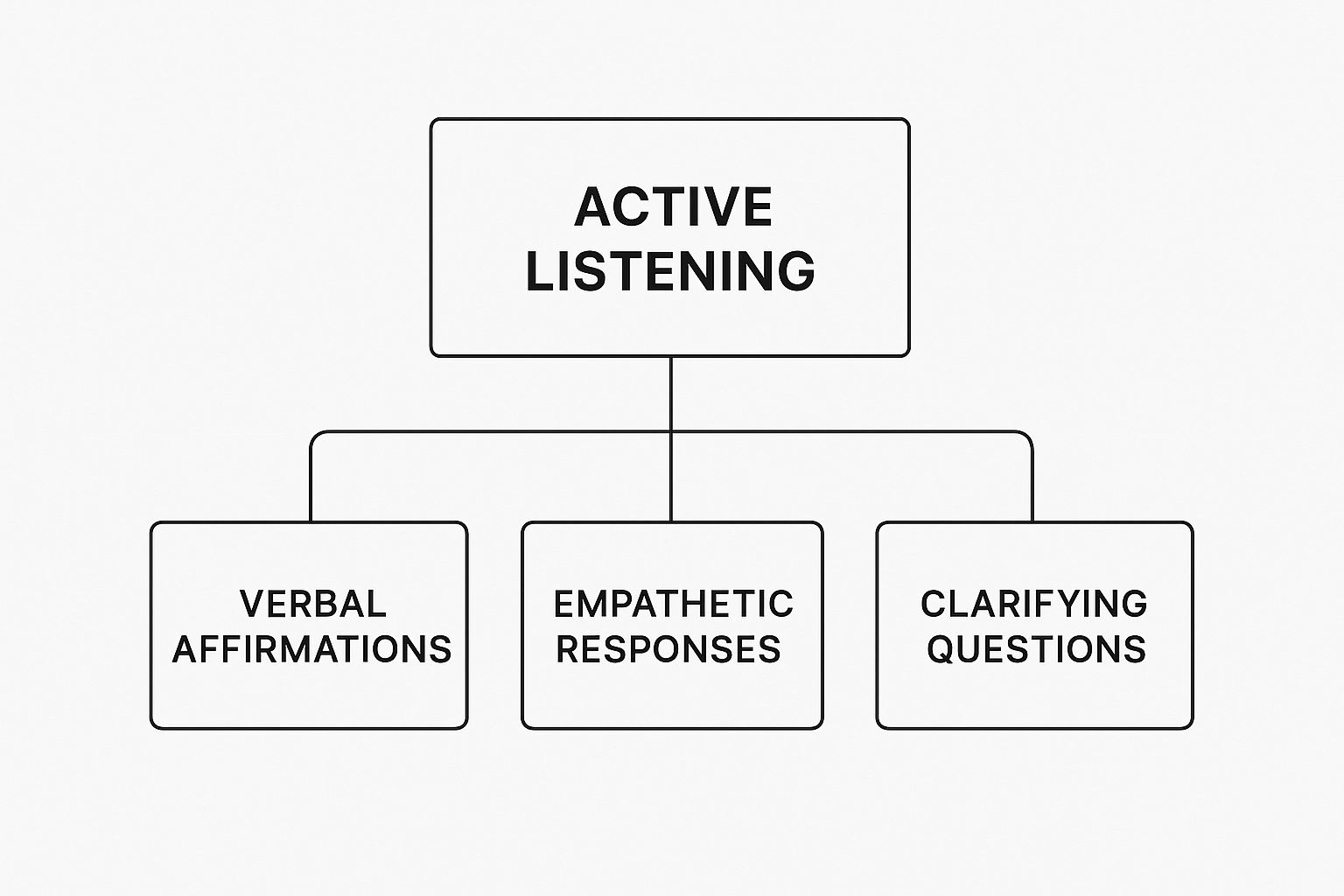
As you can see, listening isn't passive. It's an engaged process of affirming what you hear, showing empathy, and asking questions to ensure you truly understand what's being said.
To build on this foundation, we need to focus on a few key actions:
- Patient-Provider Dialogue: This is the most obvious form. It's where clinicians explain conditions and treatment plans in plain, jargon-free language. The goal is to create an environment where patients feel comfortable enough to ask questions and voice their worries.
- Team Collaboration: Just as important is the communication between healthcare professionals. Doctors, nurses, pharmacists, and therapists must share precise, timely information to coordinate care seamlessly and avoid dangerous gaps.
- Family and Carer Engagement: Involving a patient’s support network is often the key to success. Keeping family members and carers in the loop ensures the care plan is understood and followed long after a hospital visit is over.
The table below summarises these core components that form the foundation of successful communication in clinical settings.
Core Pillars of Effective Healthcare Communication
| Pillar | Description | Impact on Patient Care |
|---|---|---|
| Clarity & Simplicity | Using plain, jargon-free language that patients can easily understand. | Reduces confusion, improves treatment adherence, and empowers patients to ask questions. |
| Active Listening | Paying full attention to the patient, showing empathy, and confirming understanding. | Builds trust, makes patients feel heard, and helps uncover crucial diagnostic information. |
| Empathy | Acknowledging and validating the patient's feelings and perspective. | Strengthens the patient-provider relationship and improves patient satisfaction and cooperation. |
| Timely Information | Ensuring that communication, especially between care teams, happens promptly. | Prevents errors during handovers, speeds up decision-making, and ensures seamless care. |
These pillars work together to transform a routine interaction into a powerful therapeutic tool.
Ultimately, mastering effective communication in healthcare means recognising its power to heal, prevent harm, and forge the trusting relationships that lead to better outcomes for everyone.
Building Trust Through Patient-Centred Dialogue

Truly great communication in healthcare isn't a one-sided lecture. It's not about a clinician simply rattling off information and sending a patient on their way. It’s about creating a two-way street—a genuine dialogue where the patient feels like an active partner in their own care, not just a passive listener. This collaborative spirit is the absolute bedrock of trust.
When people feel properly heard and respected, they open up. They're far more likely to share vital details, stick to treatment plans, and ultimately, feel better about their care. The aim is to shift a consultation from a quick transaction into a meaningful interaction that builds a strong, lasting therapeutic relationship.
Shifting from Talking At to Talking With
The central idea behind patient-centred dialogue is refreshingly simple: put the patient at the very heart of the conversation. This means looking beyond the symptoms and seeing a whole person with their own unique fears, hopes, and life circumstances.
Think of it like this: any mechanic can list the technical faults in a car. A great mechanic asks where you need to go and what you rely on the car for. It’s the same in healthcare. We need to understand not just the clinical diagnosis, but the patient's personal world and what truly matters to them.
Trust is the most valuable currency in healthcare. Patients who don't trust their providers are far less likely to share the very information—both medical and personal—that could be the key to improving their health. Every small, respectful interaction helps build that trust.
This partnership approach helps the care team gain invaluable insights into a patient’s goals, their cultural background, and what’s happening in their life outside the clinic walls.
Key Techniques for Building Rapport
Forging a genuine connection doesn't have to take hours. It's about using specific, actionable techniques that show you are fully present and engaged. Weaving these into your daily practice can make a world of difference.
Here are three powerful techniques you can start using immediately:
- Active Listening: This is so much more than just being quiet while someone else talks. It’s about fully concentrating, understanding what's being said, and responding thoughtfully. Try paraphrasing their concerns back to them—for instance, "So, if I'm hearing you right, you're most worried about the side effects of this new medication." This confirms you've truly understood.
- Demonstrating Empathy: Empathy isn't about feeling sorry for someone; it's about acknowledging and validating their feelings. Simple phrases like, "That must be very difficult," or "I can see why you’d be concerned about that," show you recognise their emotional state without judgment.
- Mindful Non-Verbal Cues: Your body language often speaks louder than your words. Making the simple choice to sit down instead of standing, maintaining comfortable eye contact, and keeping an open posture can make patients feel seen and valued. In fact, studies show patients perceive that clinicians have spent more time with them when they sit down.
Ensuring Clarity with the Teach-Back Method
One of the biggest hurdles in healthcare is making sure patients actually understand their diagnosis and treatment plan. Medical information is often complex, and it’s usually delivered during a stressful, overwhelming time. This is where the teach-back method proves its worth.
Crucially, this isn't a test of the patient's memory. It’s a test of how well you’ve explained things.
After you've gone through a care plan, you simply ask the patient to explain it back to you in their own words.
It might sound something like this:
- "We've covered a lot today. Just so I can be sure I've done a good job explaining it all, could you tell me how you’re going to take this medicine when you get home?"
- "I want to make sure we're on the same page. What were the key warning signs we discussed that would mean you need to give us a call?"
If the patient struggles to explain it correctly, that’s your cue to clarify your instructions. This simple check can dramatically reduce misunderstandings, improve how well patients stick to their treatment, and empower them to manage their own health with real confidence.
Solving Common Communication Roadblocks

Even with the best of intentions, effective communication in healthcare bumps up against obstacles every single day. These aren't just abstract ideas; they're the real-world hurdles that pop up in busy clinics, crowded hospital wards, and time-crunched consultations. From navigating complex patient handovers to handling emotionally charged situations, every healthcare professional has to be a master problem-solver.
It's tempting to see these roadblocks as failures, but they're a natural part of working in such a high-stakes environment. The trick isn't to pretend they don't exist, but to have a practical toolkit ready to go. By tackling these challenges head-on with proven strategies, we can make sure information flows accurately, safely, and with empathy, protecting both patients and our own wellbeing.
Overcoming High-Pressure Situations
Time pressure is a massive barrier. When clinicians are rushed, it’s all too easy for crucial details to get missed or for patients to feel like they haven't been heard. This is especially true during patient handovers—one of the most vulnerable moments in the care journey. A messy handover can lead to serious medical errors.
This is where structured communication tools become absolutely essential. They don't just add more work; they build in efficiency and clarity right when you need it most.
Structured tools create a clear, predictable, and concise format for sharing critical information. This standardisation reduces the mental load on staff and dramatically cuts the risk of dangerous misunderstandings, especially during shift changes or transfers between departments.
One of the most effective and widely used tools for this is the SBAR framework.
The SBAR Framework: A Practical Guide
SBAR is an acronym for Situation, Background, Assessment, Recommendation. It’s a simple, four-step script that helps you get urgent patient information across clearly and quickly. Think of it as a mental checklist that ensures you don't forget anything vital in the heat of the moment.
Here’s what it looks like in practice:
- Situation: State the immediate problem. "This is Nurse Smith on Ward C. I'm calling about Mr Jones in Room 204. His breathing has become very laboured in the last 15 minutes."
- Background: Give the relevant context. "He's a 68-year-old man who was admitted yesterday for pneumonia and has a history of COPD. His last set of observations were stable."
- Assessment: Share your clinical judgement. "His oxygen saturation has dropped to 88% on room air, his respiratory rate is 30, and I can hear wheezing. I believe he's having an acute exacerbation of his COPD."
- Recommendation: Say what you need. "I think you need to come and see him immediately. While you're on your way, should I start him on nebulisers and increase his oxygen?"
Using a framework like this transforms a potentially chaotic phone call into a focused, actionable report. It makes handovers safer and far more efficient, forming a cornerstone of solid team communication.
Navigating Sensitive and Cross-Cultural Conversations
Communication gets even trickier when you're dealing with patients who are stressed, in pain, or from different cultural backgrounds. In these moments, empathy and structure are your most powerful allies.
When language is a barrier, using a professional interpreter isn't just a good idea—it's non-negotiable. Asking family members, especially children, to translate can lead to serious misunderstandings and puts them in a completely inappropriate position.
Here are a few practical tips for those difficult conversations:
- De-escalating Tense Situations: Stay calm and keep your tone of voice neutral. Acknowledge the person's feelings ("I can see you're very upset") before you try to fix the problem. That simple validation can often bring the temperature down.
- Working with Interpreters: Make sure you speak directly to the patient, not the interpreter. Use short sentences and pause often to give them time for accurate translation. Steer clear of jargon or idioms that won't translate well.
- Addressing Cultural Nuances: Be aware that things like eye contact, personal space, and who's involved in family decisions vary hugely between cultures. If you’re unsure, it’s always respectful to ask something like, "In your family, who do you normally discuss health matters with?" This shows you’re being mindful and putting the patient first.
By equipping ourselves with these strategies, we can turn those common communication hurdles into opportunities to build stronger, more trusting relationships with our patients.
Strengthening Teamwork with Better Communication

We often focus on the patient-provider relationship, and for good reason. But behind every successful patient outcome is an invisible engine: the intricate network of communication between healthcare professionals. A patient’s journey rarely involves just one person. It’s a team effort, a complex handover between doctors, nurses, pharmacists, therapists, and support staff.
When this team communicates seamlessly, care is coordinated and safe. When information gets siloed or lost in translation between shifts, the risk of error skyrockets.
Think of it like an aircraft crew. Every member has a distinct role, but they must all share a clear, unified understanding of the flight plan. More importantly, they need to feel confident enough to speak up instantly if something seems off. In healthcare, this means creating an environment where every single person feels empowered to contribute, question, and flag concerns without fear of blame. This is the very essence of a safety culture.
Fostering Psychological Safety on the Frontline
The single most crucial ingredient for strong team communication is psychological safety. This isn't a fluffy concept; it's the shared, practical belief that it’s safe to take interpersonal risks. It means feeling you can ask a "silly" question, challenge a senior colleague's decision, or admit you’ve made a mistake.
In a psychologically safe environment, a junior nurse feels just as comfortable questioning a medication dosage as a senior consultant does. This isn’t about being "nice"—it's about being effective. Hierarchy can be a killer of open dialogue in high-stakes settings, leading directly to preventable errors. Cultivating psychological safety turns every team member into an active guardian of patient wellbeing, weaving a powerful safety net.
Fostering an environment where medical staff feel comfortable speaking up about concerns or questions is paramount. This culture of transparency and collaboration is not a luxury; it is a fundamental requirement for preventing harm and ensuring the highest standards of patient care.
Building this kind of trust takes deliberate effort. Leaders must model vulnerability, actively ask for input from everyone, and respond to concerns with respect, not defensiveness.
The Power of Structured Team Communication
While a positive culture provides the foundation, structured communication practices give it a reliable framework. These aren't just meetings for the sake of it; they are targeted, efficient tools designed to get everyone on the same page, fast.
Here are a few powerful examples that really work:
- Daily Huddles: These are quick, stand-up meetings, often lasting just 5–15 minutes, at the start of a shift. The goal is simple: quickly review patient status, anticipate needs for the day, and flag potential safety issues before they escalate.
- Interdisciplinary Meetings: For patients with complex needs, bringing everyone together is vital. Getting medicine, nursing, pharmacy, and social work in the same room provides a holistic view, ensuring the care plan considers all angles and prevents conflicting treatments.
- Unified Digital Records: A shared, up-to-date electronic health record (EHR) must be the team's single source of truth. When everyone can access the same patient notes, test results, and care plans in real-time, the risk of vital information getting lost during handovers drops dramatically.
Connecting Team Dialogue to Patient Outcomes
Ultimately, strong internal communication isn't just an abstract goal—it has a direct and measurable impact on the person in the hospital bed. When a team is well-coordinated, critical details about a patient's allergies or a subtle change in their symptoms are successfully passed from the night shift to the day shift.
This seamless flow prevents dangerous gaps in care. It means a pharmacist’s warning about a drug interaction is heard and acted upon. It ensures a physiotherapist’s mobility assessment informs the nursing plan. It guarantees everyone is working from the same script. This coordinated effort is a hallmark of effective communication in healthcare, leading to safer, more efficient, and far more compassionate patient care.
How Technology is Reshaping the Conversation in Healthcare
It's a common misconception that technology is taking the human touch out of healthcare. The opposite is often true. When used thoughtfully, digital tools don't replace care—they enhance it, making the connection between a patient and their doctor more continuous and responsive than ever before. Technology is becoming a vital bridge, not a barrier.
Think about how things used to be. Communication was often boxed into the 15-minute slot of an appointment. In between visits, patients could feel isolated, and healthcare professionals had little insight into what was happening. Digital tools are now filling those crucial gaps, extending care beyond the four walls of the clinic.
This change couldn't have come at a better time, especially with the pressures facing the UK's healthcare system. We're all aware of the record waiting lists and staff shortages. Innovations like telehealth and secure messaging are no longer just 'nice-to-haves'; they're essential for delivering care, sharing information in real-time, and keeping patients engaged. For a deeper dive into this, you can find some great insights on UK health milestones and what to expect in 2025.
Making Care More Accessible and Uninterrupted
One of the biggest game-changers has been the rise of telehealth. What was once a niche service is now a mainstream reality. Video and phone consultations have exploded in popularity because they offer real, practical convenience for everyone involved.
For someone managing a long-term condition, it means a quick follow-up can happen from their living room, cutting out the stress of travel. For a new parent with a sick baby, it's about getting swift, reassuring advice without dragging everyone to a busy surgery. This is what it looks like to dismantle genuine barriers to care.
Technology extends the conversation beyond the consultation room. It creates a continuous loop of communication that helps patients feel consistently supported and allows providers to monitor progress more effectively, leading to better-managed care and stronger relationships.
Beyond video calls, other tools are making a massive difference:
- Secure Patient Portals: These give patients 24/7 access to their own health information. They can check test results on their own time, request repeat prescriptions without a phone call, or send a non-urgent message to their care team. It's about empowering people to be active partners in their own health.
- Remote Monitoring Devices: Wearable sensors and at-home gadgets are a huge leap forward. They can send a steady stream of vital signs—like blood pressure, glucose levels, or oxygen saturation—directly to a clinical team. This flow of real-world data allows clinicians to spot trouble early and step in before a small issue becomes a crisis.
Freeing Up Time Through Automation and Personalised Outreach
Another powerful benefit is technology's ability to handle the repetitive, administrative jobs that swallow up so much clinical time. Automated systems can take care of appointment reminders, send out pre-visit forms, and share educational materials, freeing up healthcare professionals to focus on what only they can do: care for patients.
This automation also opens the door to incredibly personalised patient outreach. Imagine a system that automatically sends tailored diet tips to patients with diabetes or reminds someone when they're due for a crucial screening. It’s proactive communication that keeps people engaged and on track with their care plans.
Here are a few real-world examples:
- Automated Appointment Reminders: A simple text or WhatsApp message drastically cuts down on 'no-shows,' which are a huge drain on NHS resources.
- Personalised Health Tips: A patient recovering from knee surgery could get a daily message with gentle exercise reminders or tips for managing swelling.
- Targeted Public Health Alerts: When flu season arrives, a GP practice can send vaccination reminders to all at-risk patients in one go.
Even small practices can implement these strategies using tools like WhatsApp Business. By setting it up with a service like Business Numbers Direct, they can get a dedicated professional number, separating work from personal life. From there, features like automated replies and broadcast lists make it easy to deliver the right information at the right time.
This smart blend of automation and personal touch makes communication not just more efficient, but more meaningful. It's helping to build a healthcare system that's truly connected to the people it serves.
From Multiple Channels to One Seamless Conversation
If we want to genuinely improve how we interact with patients, we need to think bigger than just having a few different communication tools. The real shift happens when we move from a multichannel setup to a true omnichannel communication strategy. It’s about creating one single, connected experience for every patient.
Think of it this way: you add a jumper to your online shopping basket, and when you open the store's app later, it’s still there. That’s the kind of seamless logic we need to bring into healthcare.
This approach means that every interaction—whether it’s a phone call, a message on the patient portal, a text update, or a face-to-face visit—is part of the same ongoing conversation. Patients no longer feel like they have to start from scratch every time they use a different method to get in touch. The system knows who they are, has their history to hand, and can pick up right where they left off.
Weaving Every Touchpoint Together
An omnichannel strategy isn't just about offering more ways to communicate; it’s about making those options work together intelligently. This is how you get smarter appointment reminders, genuinely personal health updates, and a system that actually feels like it’s listening.
Here in the UK, adopting this integrated approach is becoming less of a "nice-to-have" and more of a necessity. We're seeing healthcare organisations move away from siloed, traditional methods and towards unified platforms that pull everything—email, texts, live chat, and patient management systems—under one roof. This integration is powerful because it lets providers see the full picture of every patient's journey. You can discover more insights about healthcare communication trends on doxim.com.
An omnichannel approach ensures the patient's story is never lost. Whether they book online, call for advice, or message through a portal, their record is continuous, creating a more efficient and reassuring experience.
The Benefits of a Truly Unified System
The practical payoff of getting this right is huge. It completely breaks down the information silos that cause so much friction and frustration for patients and staff alike.
Imagine a patient gets an automated text reminder for their appointment. After the consultation, their follow-up plan appears in their patient portal. If they have a quick question later, they can ask it via a secure WhatsApp message. Each touchpoint logically follows the last, creating a smooth and intuitive flow.
This makes a healthcare practice far more:
- Responsive: Patients get the answers they need, faster, using whatever channel is easiest for them at that moment.
- Efficient: Staff aren't stuck repeating themselves or hunting for information trapped in another system.
- Patient-Centric: The entire experience is built around the patient's journey, which goes a long way toward building satisfaction and trust.
Frequently Asked Questions
Healthcare can often feel like a complicated maze, but getting a grip on good communication can genuinely light the way forward. Here are a few common questions we hear, along with some straightforward answers to help improve those crucial conversations.
What’s the Single Most Important Skill for Healthcare Communication?
If you had to pick just one, it would have to be active listening. This isn't just about hearing what's said; it's about being fully present, focusing on the patient's words, and really grasping the meaning and feeling behind them.
When you truly listen, you build trust. It shows patients they're seen and heard, which often brings critical details to the surface that might have otherwise been missed. Think of it as the foundation of any strong patient-provider relationship.
How Can Technology Improve Communication Without Losing That Human Touch?
The key is to see technology as a bridge, not a barrier. When you use digital tools wisely, they can actually strengthen human connection by making care feel more consistent and accessible. For instance, a secure messaging app lets a patient ask a quick question without the hassle of booking an appointment, while a telehealth call can make a follow-up visit much more convenient.
The aim is never to replace face-to-face conversations. It's about using technology to handle the routine stuff—like appointment reminders—so that clinicians have more time and energy for the empathetic, in-depth discussions that only a person can lead.
What Is the SBAR Technique and When Should It Be Used?
SBAR is a simple but powerful communication framework that stands for Situation, Background, Assessment, and Recommendation. It was designed to help healthcare professionals share critical patient information clearly and quickly, especially when the pressure is on.
It’s perfect for those high-stakes moments. Think of patient handovers between shifts, calling a senior doctor with a concern, or any time you need to get vital information across without missing a beat. It provides a reliable structure so nothing important gets forgotten in the heat of the moment.
How Can Patients Advocate for Better Communication?
Patients have a huge part to play in their own care. If you want to advocate for yourself or a family member, a little preparation goes a long way.
- Write down your questions and any concerns before your appointment. It’s easy to forget things once you’re in the room.
- Take notes during the consultation, or ask if it’s okay to record the audio on your phone to review later.
- Try the teach-back method yourself. You could say something like, "Okay, just so I'm sure I've got it, my understanding is I need to…"
- Never be afraid to say, "I'm sorry, I don't quite understand. Could you explain that in a different way?"
Being an active participant is the best way to make sure you walk away with the clear, understandable information you need to manage your health.
To boost your practice's responsiveness and handle patient communications like a pro, why not set up a dedicated line with Business Numbers Direct? You can get a separate WhatsApp Business number on your current mobile in minutes. This keeps your personal and professional lives apart while giving you powerful tools for patient engagement. Get your dedicated business number today.




